Treg Cellular Immunotherapy

Regulatory T cells (Tregs)
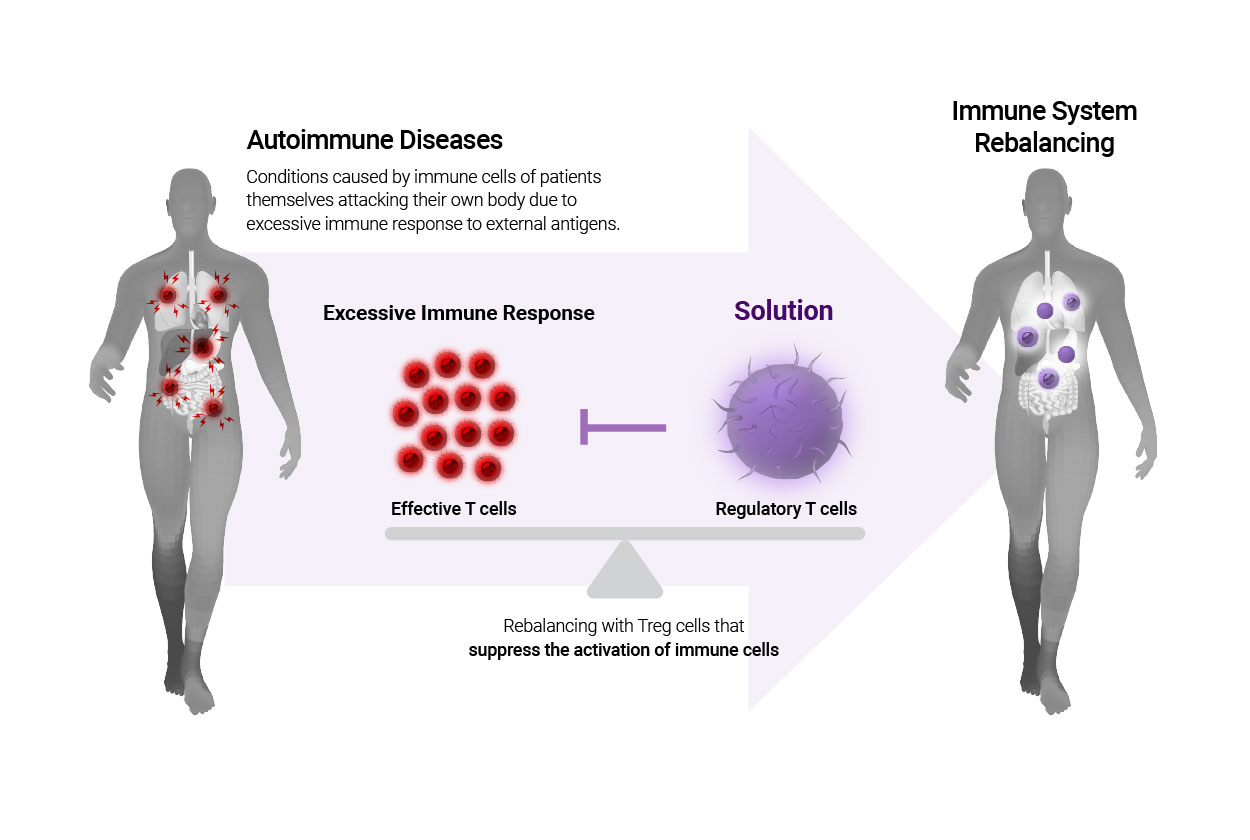
Regulatory T cells (Tregs cells) are immune cells that are dedicated to curbing excessive immune activation and maintaining immunological homeostasis with controlling immune responses from external stimulations (infection and other types of antigens). If regulatory T cells become insufficient or fail to suppress excessive immune response, autoimmune diseases may occur as the body’s defense system mistakenly attack normal cells.
Therefore, autoimmune diseases may be cured completely by re-balancing the immune system through the regulatory T cells expanded from the exterior, thereby regulating the intensity and the duration of immune responses.
Advantages of regulatory T-cells
1) Can resolve fundamental causes of diseases by restoring the balance of immune cells within the human body.
2) Fewer side effects by using cells from the human body.
3) Can expect full recovery with only a few injections due to memory function of immune cells.
Directions of R&D for utilizing regulatory T cells
Development of immune cellular therapy through rebalancing immune system
Excessive activation of immune cells is a cause of autoimmune diseases, including allergies, rheumatoid arthritis, lupus, and psoriasis. Therefore, restoring immune homeostasis that balances activation and suppression of immune responses is the most important factor in overcoming diseases related to immune systems.

Autoimmune disease
Autoimmune disease is a condition in which the immune cells that are supposed to protect our own body from external foreign substances (called antigens), such as bacteria, viruses, and other materials attack my body.
Autoimmune response may be prevalent in any organ or tissues in the human body. Endocrine organs such as the thyroid, pancreas, adrenal gland, red blood cells and connective tissues like skin, muscle, and joints are more frequently affected by autoimmune symptoms. Symptoms and conditions may vary depending on which part of the body the immune cells attack.
Existing treatments and vicious side effects
Autoimmune diseases present with a dysregulated immune response, arising as auto-reactive cells exhibiting excessive immune response attack a patient’s own body recognizing it as an intruder. Therefore, treating autoimmune diseases must involve suppressing activation, expansion and function of auto-reactive cells, but it is difficult to selectively suppress auto-reactive cells among immune cells across the whole body.
It is the reason why conventional immuno-suppressive drugs that suppress the general immune system including autoreactive cells are normally administered currently. However, using immuno-suppressants damage the functionality and reduce in the effectiveness of immune system’s response to foreign substances, so the patient should endure numerous side effects from the medication. Thus, autoimmune disease patients need to undergo long struggles against medications and their side effects, and this vicious cycle will persist until a new cure emerges.
Mechanism of action of regulatory T cells
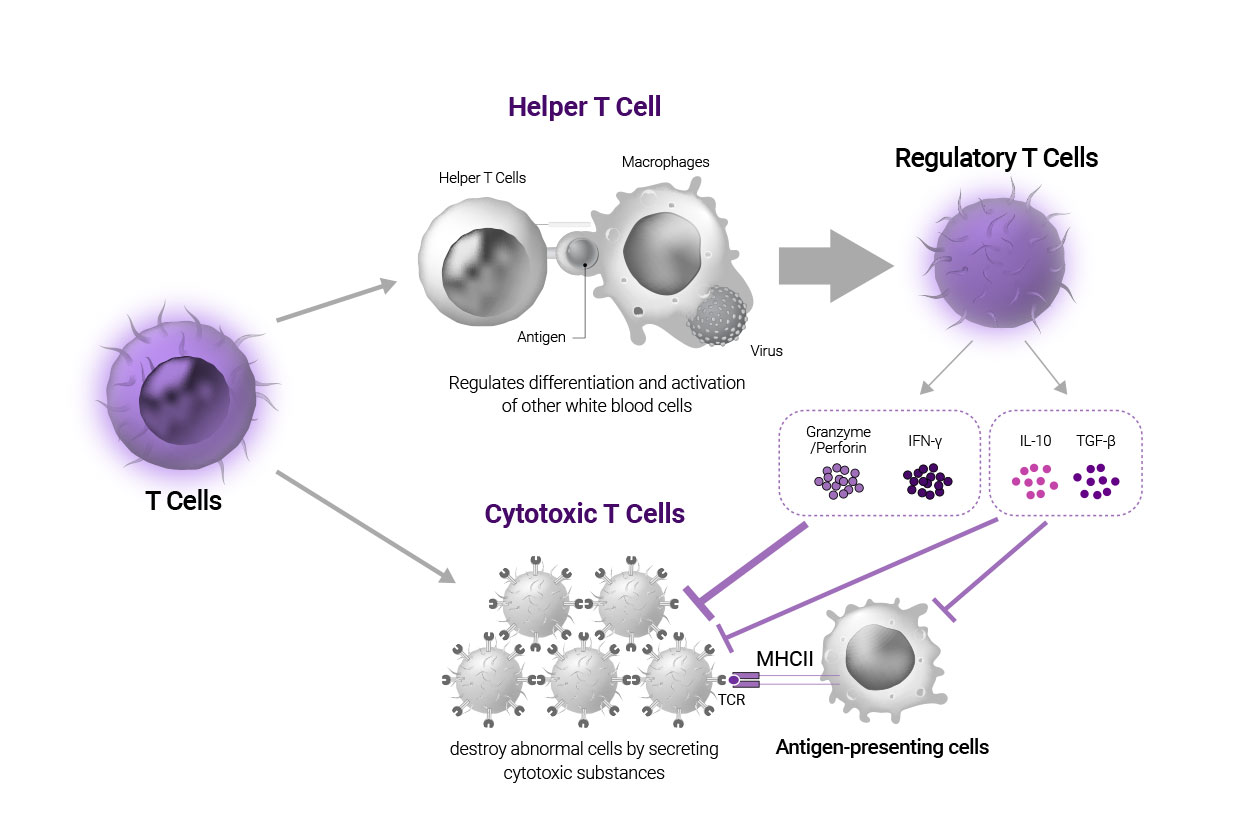
While T cells are broadly classified into helper T cells and cytotoxic T cells traditionally, different types of T cells have been discovered based on common receptors and transcription factors. Among those types, regulatory T cells (Treg cells) are known as a subtype of helper T cells. Unlike helper T cells that regulate the differentiation and activation of other white blood cells, Treg cells act to maintain tolerance toward autoantigens and suppress an excessive immune response.
They suppress the activation of T cells by taking away IL-2, which is required to activate effector T cells or secreting anti-inflammatory soluble mediators, IL-10 and TGF-β, which is triggered to suppress effector T cell indirectly and directly. Also, Treg cells secrete perforin, granzyme or INF-γ to induce cytotoxic T cells to self-terminate, and disturb antigen-presenting cells in activating other cytotoxic T cells. Hence, autoimmune diseases caused by over-activation of the immune system could be cured with cellular immunotherapeutics to achieve a rebalancing of the immune system.
You can review the information on Cellular Immunotherapy currently developing in the IMMUNIQUE laboratory.

